As we observe World Cancer Day, I want to shed light on the often-overlooked role of context in cancer care. At the inaugural Cancer Catchment Area Data Conference a few months ago, I had the opportunity to present a comprehensive overview of how geographic information system (GIS) technology is reshaping our approach to cancer care accessibility and outcomes. This blog post is an extension of that presentation, aimed at sharing the transformative impact of GIS in the realm of cancer care.
Bridging Genetics and Geography in Cancer Care
The healthcare sector frequently grapples with the nature versus nurture debate. In the context of cancer care, this might translate to a comparison between genetic code and ZIP Code – with the latter serving as a metaphor for all types of locations. While the focus of cancer research has been on bench science, uncovering the minute interactions and patterns related to diagnostics and therapeutics, it’s crucial to acknowledge both elements. The scientific community has achieved remarkable breakthroughs, such as positron emission tomography (PET), X-ray computed tomography (CT), magnetic resonance spectroscopy (MRS), and various molecular diagnostic techniques, along with advancements in therapeutics like CRISPR, immunotherapies, robotic surgery, and artificial intelligence. These developments are indeed groundbreaking.
Yet, the accessibility of these innovations is not universal. The cumulative lifetime of exposures that each individual encounters, potentially contributing to cancer development, is a facet yet to be thoroughly explored. Additionally, the challenge of facilitating collaboration and scaling research efforts persists. Here, and in other ways, GIS plays a pivotal role with its inherent capability to collect, visualize, analyze, and apply geographic data. Such an approach is instrumental in supporting cancer centers across seven key areas, significantly enhancing the efficacy and in fact, the equity of cancer care.
1. Defining Catchment Areas with Precision
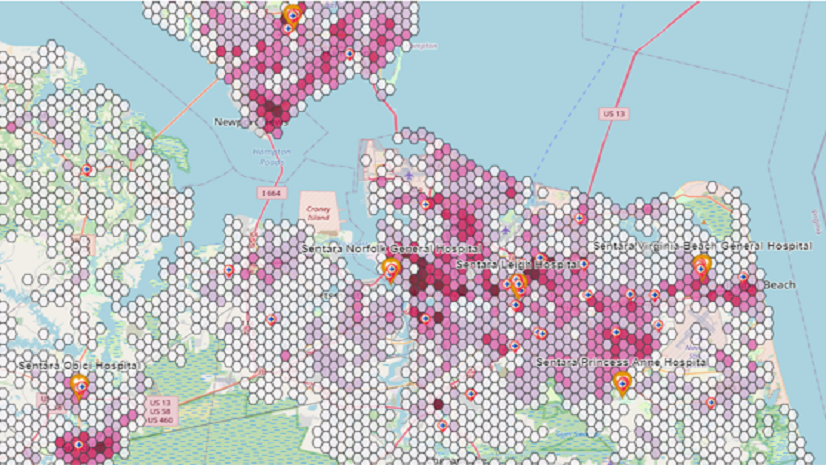
The first step in cancer care accessibility is accurately defining catchment areas. Traditional methods using straight-line distances from ZIP Code centroids can ignore real-world obstacles like topographical barriers (e.g. lakes, rivers, mountains), which can mask access disparities. GIS aids in overcoming these challenges, using road network data and drive-time calculations to provide a more accurate representation of access.
Once a catchment area is established, GIS supports ‘geo-enrichment’ – characterizing the population within these boundaries. This process includes understanding the cancer burden, demographic makeup, and special characteristics that might hinder accessibility, such as disabilities or conditions requiring frequent treatments, such as daily radiation therapy.
2. Assessing Needs and Directing Resources
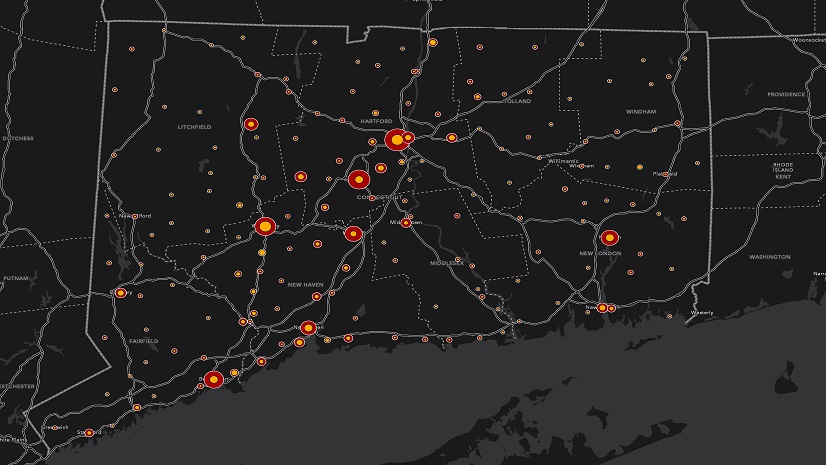
GIS also plays a vital role in performing in-depth community health assessments and resource inventories for cancer-related programs. By identifying assets and gaps, these tools help direct new resources more effectively, ensuring that every patient receives the care they need.
3. Engagement and Decision-making Tools
For inclusive decision-making, GIS offers tools for surveys and sentiment analysis. An illustrative example is the ALS Clinic survey developed by Sandy Morris and Pat Dolan. Although this survey is focused on a different devastating disease, it has already provided valuable insights into patient experiences while highlighting areas for improvement in clinic performance.
4. Addressing Disparities with Data-Driven Insights
Mapping outcomes and tracing upstream factors like community conditions and policies is essential in both exposomic research (research that examines environmental exposures and their impact on health) and addressing disparities in cancer care. As practical example, many organizations used GIS to correlate low vaccination rates with social vulnerability, leading to targeted interventions and improved vaccine uptake.
5. Clinical Trial Representation and Accessibility
GIS also facilitates better clinical trial participation empowering both patents and providers. Imagine the ability to quickly connect patients and providers with relevant clinical trials, searching by patient and cancer characteristics as well as location, enhancing accessibility and participation.
6. Research to Policy Translation
Maps move people. GIS has been used to support various health policy decisions such as social distancing guidance during the height of the COVID-19 pandemic, fast-tracking drugs for rare diseases into use, and updating statewide vaccine policies. I’ve no doubt that GIS can support the translation of cancer research into policy development and adoption as well.
7. Extending Research Reach through Public Dissemination
Public dissemination of information and facilitating collaborative opportunities is another area where GIS shows its strength. The Dana Farber Institute’s StoryMap on Massachusetts’ cancer data exemplifies how GIS can be used to share cancer statistics interactively and provide valuable resources for patients and researchers alike.
We’ve also seen the undeniable power of GIS in fostering real-time collaboration. The National Interagency Fire Center’s GIS-hub for wildfire management is a testament to the capability of GIS in connecting hundreds of organizations and disseminating real-time information.
The Power of Location in Decision Making
Understanding context or location is vital in viewing the world holistically, with clarity and making informed decisions in cancer care. As we commemorate World Cancer Day, let’s be grateful for the advancements happening on the ‘nature’ side of the debate and embrace the potential of GIS to do its part supporting the ‘nurture’ side. Location intelligence will transform cancer care, ensuring accessibility and improving outcomes for all.
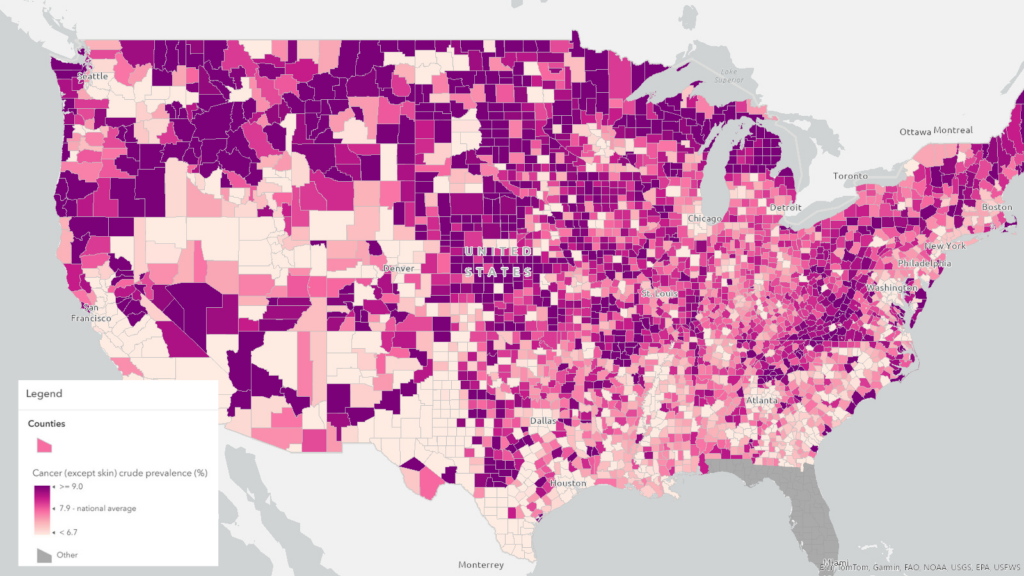
Incorporate the power of location into your decision making today by accessing the above complimentary web map in ArcGIS Living Atlas of the World. Or learn more in Dr. Geraghty’s peer-reviewed article.