Most recent
Dayton Fire's Unified Command Using ArcGIS Mission
Dayton Fire Department has embraced cutting-edge GIS to enhance its operational efficiency during special events and for disaster response.

Esri Brings Next-Gen Public Works to PWX 2025

Madison Musgrave|
Mapping Open Spaces for Disaster Response

Facsa’s GIS Journey: From Paper Maps to a Spatial Digital Twin

On the Way to the Connected Digital Twin: DB Systel Relies on GIS and Location Services

Empowering the Future of Environmental Consulting with Geospatial Innovation

Rebecca Kahrhoff|
Mapping for Mine Closure: Why GIS is the Key to Sustainable Reclamation

Headed to APWA’s PWX? Stop by Esri to Learn How Next-Generation Public Works is Powered by ArcGIS
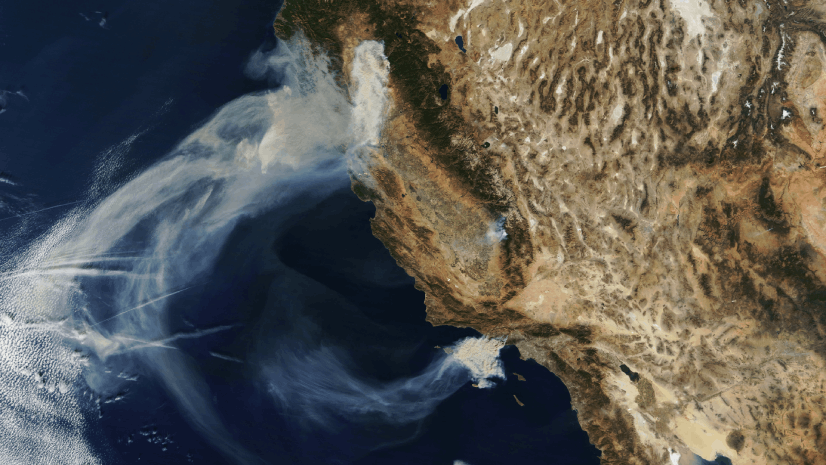
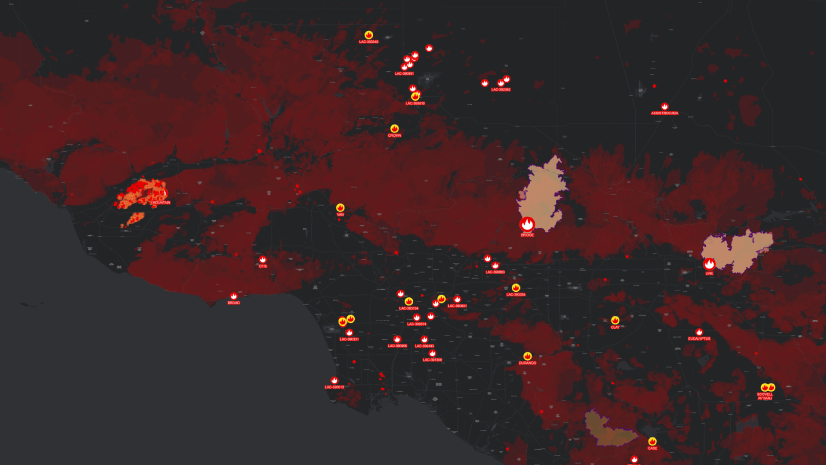
Seeing the Big Picture: Remote Sensing in the Wildfire Technology Toolkit

Showrooming: At a Grocer Near You.

ICSC Las Vegas 2025: Retail’s Data-Driven Evolution

GIS-Powered Precision at Great River Energy: Fault Location Transformed